Experian Health announced it has acquired MyHealthDirect, a SaaS-based company specializing in digital coordination solutions in scheduling.
We interviewed Jason Considine, Experian Health general manager of patient engagement and collections, to learn more about the acquisition, as well as opportunities arising in healthcare due to the rise in consumerism.
What led to Experian’s interest in MyHealthDirect and the ultimate acquisition?
We’ve had a relationship with MyHealthDirect for several years. Experian Health has been reselling the MyHealthDirect solution since 2017, and we’ve long recognized that their platform’s digital care coordination capabilities would be a great match with our existing solutions. MyHealthDirect’s platform links patients with the right providers, offering online scheduling tools and referral coordination to ensure more timely access to care for patients. These solutions have proven to increase appointment and referral rates, improve call center efficiency, reduce no-shows and enhance the overall patient experience. By coupling this technology with our Experian data, we can ensure patients are getting the care they need in the management of chronic diseases and wellness programs. This acquisition evolves our core revenue cycle management capabilities and helps us make gains in the patient engagement space with all-new innovative offerings.
You referenced “digital care coordination.” What does this mean and how does it apply to healthcare?
Digital care coordination, as it applies to the MyHealthDirect suite, is comprised of self-scheduling, call center, referral coordination and automated outreach solutions, making it easier for people to access healthcare. By combining these scheduling solutions with Experian’s existing digital patient engagement solutions, we can deliver a seamless consumer-centered experience – from serving up an estimate, to streamlining the registration process, to providing consumers with the ability to pay their healthcare bills via multiple channels.
Today’s healthcare consumer expects a turnkey, personalized, on-demand experience. When you think about the best engagements we all enjoy in retail, financial services, travel and entertainment, the expectation is that the healthcare experience should be no different. We need to arm consumers with the ability to streamline their healthcare and make it easier for them to access care.
Why is the scheduling component so key in the overall patient journey today?
Scheduling is the one of the very first steps of the care journey and booking an appointment has traditionally been a poor experience. Common frustrations include not being able to reach the provider, finding out that no appointments are available, or being forced into a time-consuming three-way call between the health plan and provider. Without fast and easy access, patients may not be able to get the care they need. When healthcare plans use technology to better connect patients to needed care, quality scores for patient experience rise and efficiencies are gained.
Can you give us an example on how more automated approach to scheduling could lead to better health outcomes for the consumer?
Sure. Take for instance an individual who is living with diabetes. It is important for this person to have regular check-ins with their provider to monitor their condition and adjust care plans accordingly. If this person is challenged to see their provider, or doesn’t have regular appointments booked, they could run the risk of becoming an unhealthy diabetic, being faced with additional health challenges. By tapping into digital appointment scheduling, a provider or payer could create an automated outreach plan to make the scheduling hassle-free. Appointments could be streamlined and scheduled directly on the phone via IVR or text, and appointment reminders can be delivered.
How do you see providers responding to the rise in healthcare consumerism?
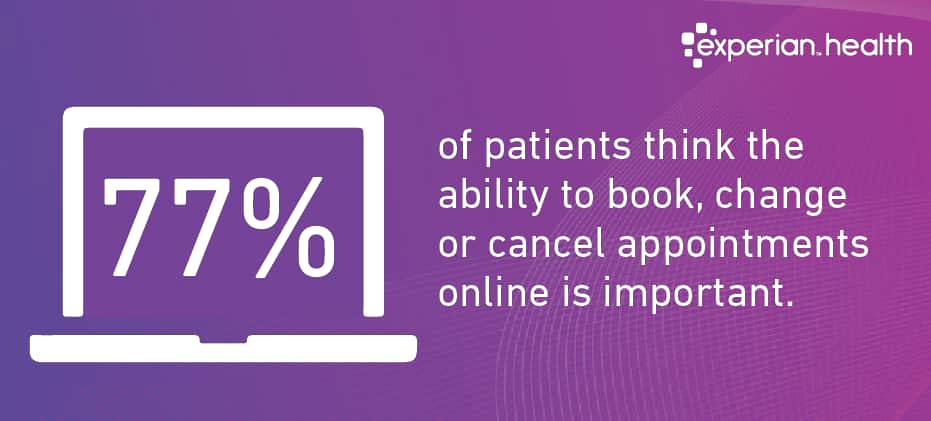
It’s no secret that healthcare costs are rising, and consumers are increasingly bearing more of those costs. Providers, therefore, are telling us they need to deliver a better experience. They are asking for digital technologies to gain rich insights into consumer behavior and then adjusting their care delivery plans accordingly. They recognize that consumers have a choice on where to take their healthcare business, so they need to compete. In the case of scheduling, MyHealthDirect conducted some research and revealed 66% of patients would switch providers for more convenient access. In that same study, 77% of patients think the ability to book, change or cancel appointments online is important. My point? Those providers and payers investing in on-demand tools to interface with their consumers will win, simplifying many of the administrative tasks associated with healthcare.
—
Learn more about scheduling solutions.


