Dayton Children’s Hospital is a pediatric hospital in Ohio with over 300,000 annual patient visits. Ranked by U.S News & World Report as one of the top 50 pediatric facilities in the United States, the facility’s mission centers around providing “optimal health for every child.”
Challenges
The Patient Accounts department, led by Richard Gonzales, wanted to reduce his team’s reliance on third-party collections agencies and avoid associated fees. This meant that his in-house team needed to further scale its operations and processes to reach their in-house collections goals.
The Pre-Service Operations department, managed by Jason Schenck, pursued efficiencies for resources within the centralized scheduling team, including the goal to quickly respond to referrals and turning those referrals into scheduled appointments within 24 hours.
Throughout the pandemic, both teams experienced staffing shortages and pandemic-related absences. Because their dialing methodologies were manual, these disruptions in personnel prohibited them from growing in-house collections and reaching the turnaround times Schenck’s team wanted to achieve for scheduling referrals.
As Dayton Children’s strived to achieve these ambitious goals, they decided to proactively provide a better patient experience through convenience, connection and an effective communication experience.
Resolution
Dayton Children’s launched Experian Health’s PatientDial solution in the Patient Accounts department to scale their in-house collections efforts, thereby reducing dependency on their outside collections agencies.
The solution was also adopted in the Pre-Service Operations department to automate dialing and conversation readiness so that the team could expedite the scheduling of referred patients.
The expertise of a dedicated Experian Health consultant provided unwavering support to the two departmental heads and also gave them full control over the operations to best match their expectations.
Streamlining patient payment collections with PatientDial
The Patient Accounts department’s operations revolve around billing a claim, reducing bad debt, increasing patient collections and providing effective customer service. They devised a two-pronged approach when it came to contacting patients for payments. The outbound campaign focused on collections, whereas the inbound customer service team handled the large volume of incoming calls from customers and rerouted them to the correct department.
When it comes to collections, the Patient Accounts department found that making phone calls was the most effective medium to support their collections efforts. Billing is a complex process and taking the time to connect with patient guarantors to explain those bills paid off.
To refine the communication approach, patient accounts were segmented based on outstanding balance amounts and where they were on the statement cycle. Calls were then made to the accounts with the highest propensity to pay.
Waiting on hold not only wastes a patient’s time but also leads to a frustrating patient experience. Many even abandon calls, to call again later, which makes phone lines even busier. To provide a better patient experience, the department was also able to try out an innovative recall campaign, enabled by the queue callback feature. Patients were called back automatically the moment an agent became available, thereby reducing call hold time. By providing patients with this callback option, Dayton Children’s is empowered to accept more inbound calls per day along with having empathetic conversations with guarantors around payment plans to sustain its collections goals.
Patient scheduling and preregistration powered through automation
The Pre-Service Operations department leveraged PatientDial to improve outbound call efficiency and optimize existing staff resources to schedule appointments rather than leave voicemails. The productivity for scheduling a new patient visit from an outbound call was about 30%. With the centralized team supporting more than 40 specialty clinics, the team needed to improve the number of new patient visits scheduled daily, which meant opening resources to receive inbound calls. The mighty team of 10 was able to strategically use the autodialer feature to make new appointments, send appointment reminders and schedule referrals.
Time is of the essence in a healthcare setting, and swift access to pertinent patient information enabled the staff to start their work even before greeting the callers when an inbound call came. Powered by the agent pop feature, staff had immediate access to key patient identifiers such as name, date of birth and specialty clinic from referral. Additionally, the feature enabled the team to reinvest time in creating a positive patient experience through improved hold and talk times, both of which reduce the risk of call abandonment.
Results of incorporating PatientDial
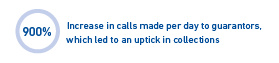
With PatientDial, the Patient Accounts department has been able to successfully align revenue goals with employee productivity. Previously, the staff was able to make only 50–60 calls per day, out of which 70% went unanswered. By automating dialing, the staff is now able to make 600 calls per day, resulting in a corresponding uptick in collections. The recall campaign, used for following up with patient guarantors, was a new endeavor for the department and has reduced the staff’s burden of making 300 manual calls per day and has also reduced call abandonment rates.


The Pre-Service Operations department, has seen a 50% increase in patient appointments scheduled, powered by 600–800 automated calls made per day. The referral-to-scheduled appointment timeline has gone down from 4 days to under 1 day. Two hundred patients can now be reached via text daily and the speed to answer calls has been reduced from 60 seconds to 30 seconds.
Lastly, PatientDial has positively challenged the Pre-Service Operations department to rethink productivity and daily operational efficiency.



Dayton Children’s investment in dialing automation has streamlined their patient communications around scheduling and far exceeded initial goals. Because of the resulting high volumes of new patients scheduled and improved efficiency and effectiveness the team realized, there’s a strategic plan specific to central scheduling and to implement standard processes for managing new patient referrals across the organization.
What’s next for Dayton Children’s?
Empowered by their stellar results, both the Patient Accounts and Pre-Service Operations departments want to further explore how PatientDial could help other departments achieve greater productivity and further deliver a positive patient experience.
The Patient Accounts department wants to maintain its focus on productivity gains and employee experience through PatientDial, with the ultimate goal of bringing in more collections.
The Pre-Service Operations department plans to take on additional scheduling responsibilities across departments, creating time to reinvest in direct patient care and improving patient outcomes. Initial plans are for establishing patient scheduling and improving processes to identify and schedule follow-up visits.
Both the teams at Dayton Children’s recognize Experian Health’s expertise in revenue cycle solutions, which has made this a successful partnership.
Learn more about how PatientDial uses patient outreach and patient engagement processes and workflows to increase your bottom line.


